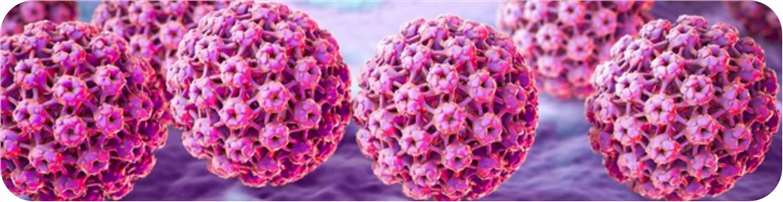
Human papillomavirus (HPV), a common sexually transmitted infection, can beget a wide range of health problems including genital warts and cancers. Development of HPV vaccine is a major advance in guarding people against the contagion. The first HPV vaccine, Gardasil, was approved by the US Food and Drug Administration (FDA) in 2006. This vaccine protects against several HPV strains (e.g., 6, 11, 16, and 18) known to induce cervical cancer and genital clods.
The development of HPV vaccines is a complex and grueling process that requires time for exploration and testing. Researchers must identify specific HPV strains that are most likely to trigger cancer and develop a vaccine that stimulates the immune system to produce antibodies against those strains. Ensuring the safety and efficacity of HPV vaccines is a significant challenge in their development. Like all vaccines, HPV vaccines must undergo expansive clinical trials to prove their safety and effectiveness. These trials involve typically thousands of subjects and require considerable time. One of the major improvements in the development of HPV vaccines is a technology called virus-like particle (VLPs), which are molecules that resemble the structure of viruses but don’t contain the complaint-causing viral genetic material. This allows the immune system to respond quickly and click out the virus when facing an attack.
Research and development of HPV vaccines has been ongoing since the early 2000s, with multiple clinical trials demonstrating the safety and efficacity of the vaccines. The vaccines have been shown to be largely effective in precluding HPV infection and related conditions, with some studies reporting a 90% reduction in HPV-related cancers in vaccinated individualities. In recent times, efforts have been made to ameliorate the availability and vacuum degree of HPV vaccines, particularly in low-income countries where cervical cancer is a leading cause of cancer-related deaths. In addition, enterprises similar as the Global Alliance for Vaccines and Immunization (GAVI) have helped to increase the distribution of HPV vaccines to these regions.
Future explorations in HPV vaccines may include the development of thermostable formulations that are not required for refrigeration, as well as the possibility of vaccination programs targeting older age groups and males to further reduce the burden of HPV-related disease. In addition, novel vaccine delivery systems, such as DNA-based vaccines and nanoparticle-based vaccines, are currently being investigated and could potentially improve the efficacy and availability of HPV vaccines.
Overall, the development of HPV vaccines has been a major cornerstone of the fight against HPV. Continued researches and efforts are needed to ensure that these vaccines reach all populations at risk of HPV-related disease. The future of HPV vaccine research and development is promising, as advances in technology and an increasing understanding of the virus will provide the basis for new innovations in vaccine design and delivery.