Starting off:
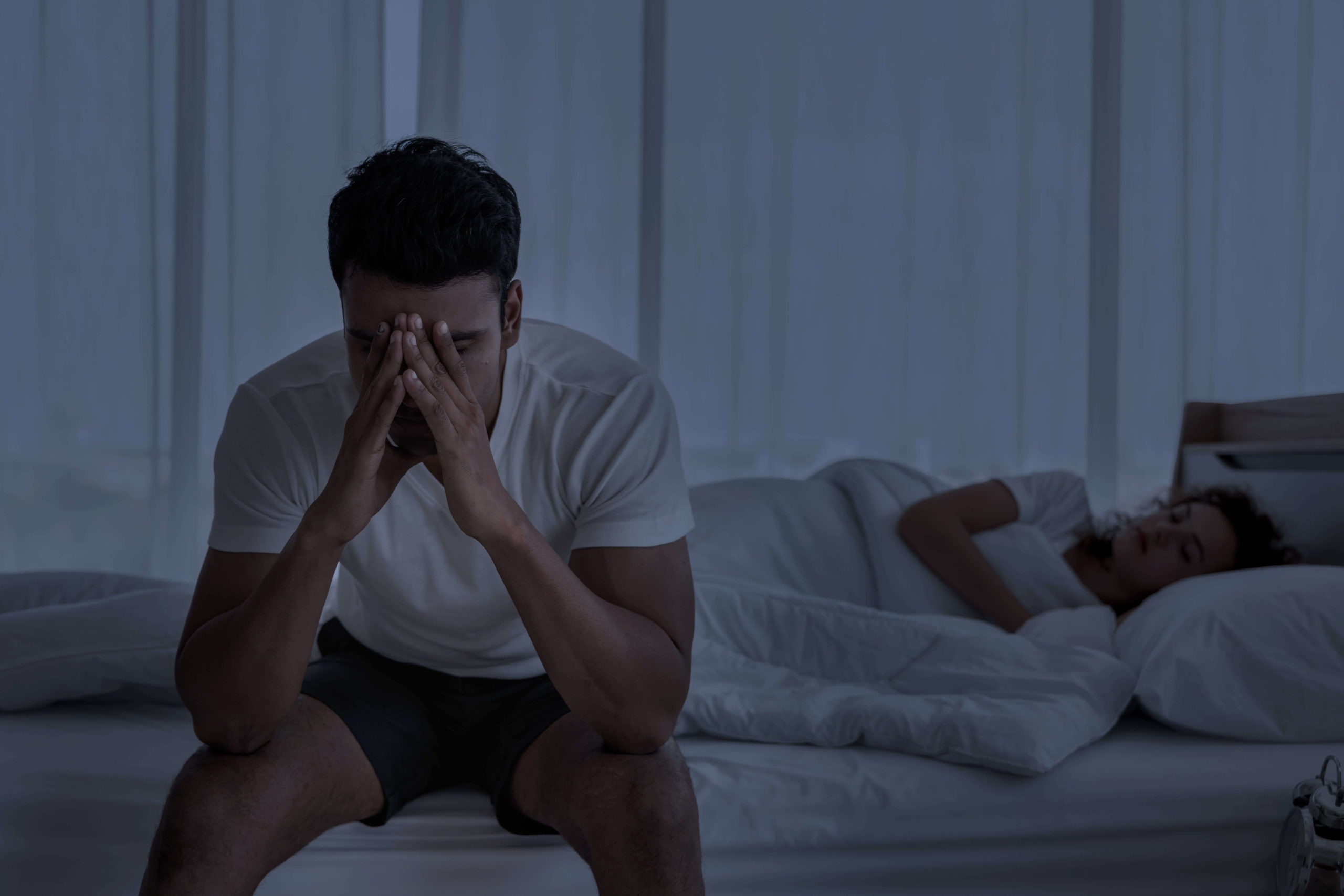
Individuals who are in constant pain often have trouble sleeping. Each makes the other worse, so the link between pain and sleep goes both ways. Chronic pain can make it hard to sleep, and not getting enough sleep can make the pain worse. This piece will talk about how to deal with insomnia in people who have painful conditions and the complicated relationship between chronic pain and sleep disorders.
Understanding Chronic Pain and Sleep Disorders:
Chronic pain is pain that doesn’t go away after a regular amount of time for healing from an illness or injury. It usually lasts for three to six months or longer. It may be caused by a number of diseases, including arthritis, fibromyalgia, back pain, neuropathy, migraines, and more. Not only does chronic pain hurt your body, it also has a big effect on your mental health and quality of life.
Insomnia, sleep apnea, restless legs syndrome (RLS), and periodic limb movement disorder (PLMD) are all sleep problems that are common in people with chronic pain. People who have chronic pain are more likely to have insomnia, which means they have trouble going asleep, staying asleep, or getting restful sleep. Pain can mess up the structure of sleep, which can lead to broken sleep and worse sleep quality.
Things that make it hard for people with chronic pain to sleep:
Several things can make it hard for people with severe pain to sleep:
Pain Intensity:
People who have chronic pain may have trouble falling asleep and staying asleep depending on how bad their pain is. When you’re in pain all the time, it can be hard to find a good position to sleep in and stay in that position all night.
Psychological Factors:
Anxiety, sadness, and stress are all conditions that often happen along with chronic pain and can make sleep problems worse. Arousal from negative feelings and thinking can make someone hyperaroused, which makes it hard for them to calm down and fall asleep.
Medications:
Opioids, antidepressants, and anticonvulsants are some of the medicines that doctors recommend to treat chronic pain that can make it hard to sleep. Side effects like sleepiness, insomnia, and drowsiness during the day may make it harder to get enough sleep.
Sleep Environment:
Things outside of the bed, like noise, light, temperature, and uncomfortable clothing, can also make it hard for people with chronic pain to sleep. Making a sleep-friendly setting is important for getting the best sleep possible.
Taking care of insomnia in people with chronic pain:
People with chronic pain need a multimodal approach that treats both the pain itself and the sleep problems in order to effectively manage their sleeplessness. Here are some ways to help people with severe pain deal with insomnia:
Pain Management:
Comprehensive pain management plans that try to lessen the severity of pain can improve the quality of sleep. Medications, physical therapy, cognitive-behavioral therapy (CBT), acupuncture, and mindfulness-based methods may all be part of this.
Sleep Hygiene:
Teaching people good sleep hygiene habits is an important part of encouraging healthy sleep habits. This means sticking to a regular sleep routine, making sure your bedroom is comfortable, staying away from caffeine and activities that wake you up before bed, and learning how to relax.
Cognitive behavioral therapy (CBT) for insomnia: The cognitive behavioral therapy (CBT-I) method to treating insomnia is structured and based on research. Its main goal is to change unhealthy beliefs and behaviors about sleep. It includes methods like controlling stimuli, limiting sleep, learning how to relax, and changing the way you think.
Mindfulness-Based treatments:
Mindfulness-based treatments, like mindfulness meditation and mindfulness-based stress reduction (MBSR), have been shown to help people with chronic pain sleep better and feel less pain. These activities help you relax, stop dwelling on negative thoughts, and accept your pain better.
Pharmacotherapy:
Because of the risk of side effects and addiction, medications should only be used with care in people with chronic pain. However, some medications may be given to help people who have trouble sleeping. Some examples are non-benzodiazepine hypnotics, tricyclic antidepressants, and low-dose antidepressants that make you sleepy.
Interventions Related to Sleep:
Patients with chronic pain and sleep apnea may benefit from continuous positive airway pressure (CPAP) therapy. Dopaminergic drugs or alpha-2 delta ligands are two treatments for RLS and PLMD that can help ease symptoms and make sleep better.
Collaborative Care: It is important for pain specialists, sleep medicine specialists, psychologists, and physical therapists to work together in order to really help people with chronic pain and sleep problems. A multidisciplinary method lets treatment plans be made just for each person, based on their specific needs.
In conclusion:
People who are in constant pain are more likely to have sleep problems, which makes their physical and mental health even worse. Managing insomnia in people with chronic pain needs a comprehensive method that takes into account both pain management and sleep problems. As part of multimodal interventions like pain management, sleep hygiene, cognitive-behavioral therapy, mindfulness-based interventions, pharmacotherapy, and collaborative care, healthcare workers can help this group sleep better and feel better overall. Giving patients the information and skills they need to control their sleep well can make a big difference in their quality of life and ability to function.